Refractory Ventricular Fibrillation
Management of Refractory Ventricular Fibrillation
Recently, some of my wonderful colleagues at Tampa General had a patient brought in via EMS in “refractory ventricular fibrillation”. Upon arrival to the ED, the decision was made to attempt double sequential defibrillation as well as initiate esmolol. Remarkably, the interventions were a success and today the patient is alive and well.
This incredible outcome prompted the question, “How much evidence is there behind the decision to attempt double sequential defibrillation and initiate esmolol?” To my surprise, there is very little data available. While there are a number of case reports floating around for each of the two topics, in both cases I found only a small handful of larger-scale studies, most of which are retrospective and still quite tiny in sample size. With that in mind, we will discuss these topics a little more. This particular post will focus on double sequential defibrillation.
What is Refractory Ventricular Fibrillation?
Although a universally accepted definition does not exist, the most commonly accepted definition is ventricular fibrillation that has persisted after three attempts at defibrillation. Because ventricular fibrillation is commonly receptive to defibrillation, it is thought that the underlying pathophysiology of refractory ventricular fibrillation is likely different from ventricular fibrillation that is receptive to defibrillation. Refractory ventricular fibrillation is thought to be associated with high levels of sympathetic hormones as well as high intracellular calcium levels which contribute to the refractory nature of the disease state, making it more resistant to attempts at defibrillation. As a quick aside, as there is some thought that elevated intracellular calcium might be contributory to the disease process, it is reasonable to at least consider forgoing intravenous calcium in this patient population unless there is concern for hyperkalemia.
Double Sequential Defibrillation
When we’re talking about double sequential defibrillation, we mean placing a second set of pads in the anterior posterior position in addition to your normal anterior-lateral positioning. In the anterior-posterior position, one pad is placed on the anterior chest between the two antero-lateral pads, and the other pad is placed directly posterior to it on the patient’s back. With both sets of pads in place, you then charge both sets and fire one immediately after the other (not simultaneously). Really what we care about here is successfully defibrillating the left ventricle, and so there are a few proposed hypotheses for how this may help:
Hypothesis 1: The extra energy is more likely to succeed than with one set of pads.
Hypothesis 2: It is the change in the vector that’s most important, in that the anterior-posterior positioning is a much more direct current to the LV.
Hypothesis 3: The cardiac tissue somehow becomes primed by the first shock, making the second more effective.
All these hypotheses are speculative, and the true underlying pathophysiology may be some combination of the three (or perhaps even none at all). With respect to the above hypotheses, the hypothesis regarding the “vector change” benefit supports the notion that the ideal placement of the second set of pads is as described above (one anterior, one posterior, with our heart essentially squarely in the middle of the two). With the left ventricle being the most posterior portion of the heart, the change in vector should optimally reach through the ventricle in a way that our standard placement is much less likely to do. With all that said, getting a defibrillator pad onto the patient’s back in the middle of a code, while trying to perform high quality CPR, is not the easiest task. As such, an acceptable alternative, though probably not ideal, is termed the anterior anterior placement. In this version, both pads will be placed on the anterior portion of the patient’s chest. The first pad will be just medial to your typical anterior pad, and the second pad will be just superior to your typical lateral pad.
Do We Have Data on Double Sequential?
Double sequential external defibrillation for refractory ventricular fibrillation: The DOSE VF pilot randomized controlled trial
Cheskes S, Dorian P, Feldman M, et al. Resuscitation. 2020;150:178‐184.
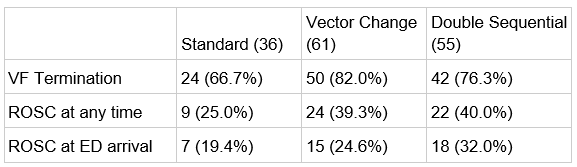
The first study we’ll look at is the only randomized control trial that we have on the subject. In this case, it’s a pilot RCT that took place last year: the DOSE VF pilot RCT. The full randomized control trial is on the horizon, so for now we just have this early data. In this pilot RCT the authors divided patients into three arms: standard, vector change (which is just one set of pads using the alternative anterior-posterior positioning), and double sequential. Take note that by pure chance fewer patients were in the standard group, due to the randomization being for set lengths of time.
The results, however, seem promising for both vector change and double sequential defibrillation, with improved rates of VF termination and rates of ROSC. Interesting to note that double sequential didn’t seem to add anything over the vector change. This could throw some early support to the hypothesis that the vector change is primarily driving any benefit from double sequential defibrillation, but at this point it’s just too early to know. Perhaps the biggest weakness in this study is the lack of any patient-centered outcome, preventing us from having any idea if there was any improvement in mortality or neurologically intact survival. Overall, our only RCT looks quite promising, with the full RCT coming. However, before we get too excited, let’s look at how the prior literature on the topic appeared.
Prehospital double sequential defibrillation: a matched case-control study
Mapp JG, Hans AJ, Darrington AM, et al. Acad Emerg Med. 2019;26(9):994-1001.
The next paper we’re looking at is a paper by Mapp et al from 2019. In this paper they set up a program that allowed EMS to decide to use double sequential defibrillation if they thought that it was appropriate. In the end they wound up with 64 cases of survivors to hospital admission, which they then subsequently matched to 64 cases of individuals who did not survive to hospital admission. Of the 64 survivors, 12 received DSD. Of the 64 non-survivors, 13 received DSD. They then subsequently compared standard defibrillation with DSD.
Overall, the double sequential group looks quite poor to the standard defibrillation group. However, it is important to bear in mind that the methodology of this paper does make it possible for a selection bias to be influencing the results. We do not know why EMS decided to use double sequential defibrillation on certain patients and not on others. Nevertheless, this paper is a firm negative in terms of positive benefit from the double sequential intervention.
Effectiveness of Prehospital Dual Sequential Defibrillation for Refractory Ventricular Fibrillation and Ventricular Tachycardia Cardiac Arrest
Lauren R. Beck, Daniel G. Ostermayer, Joseph N. Ponce, Saranya Srinivasan & Henry E. Wang Prehospital Emergency Care. 2019; 23:5, 597-602.
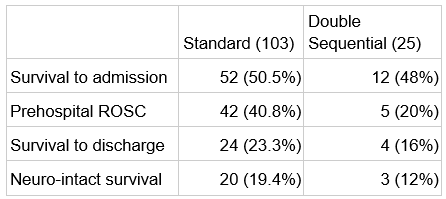
Next paper: Beck et al, also from 2019. This one was a retrospective review from the Houston EMS system. Data is shown below, and as you’ll be able to see pretty quickly, not very promising for double sequential.
Double sequential performed more poorly than standard defibrillation in every variable measured, by decent margins in most cases. Again, we have to bear in mind, however, that this is retrospective data and as such we cannot claim to know exactly why some got double sequential and others did not. Nevertheless, another clearly negative study.
The impact of double sequential external defibrillation on termination of refractory ventricular fibrillation during out-of-hospital cardiac arrest
Cheskes S, Wudwud A, Turner L, et al. Resuscitation. 2019;139:275-281.
The next paper is another by Cheskes et al, also in 2019 (same leading author as our pilot RCT above). This paper was another retrospective review, this time using prospectively collected data for a different original purpose.
With the key outcomes being studied here as rates of VF termination and ROSC, this study represents another negative for double sequential, having slightly worse rates in both categories than its standard counterpart. Interestingly, the authors break down their study into shock-based analysis, arguing better rates of VF termination for both early (attempts 4-8) and late (attempts after 8) defibrillation. Despite this, given that the overall rate of VF termination is still lower in the double sequential group, it is hard to put much stock in those analyses.
Double Sequential Defibrillation Therapy For Out-of-Hospital Cardiac Arrests: The London Experience
Emmerson, A.C., et al, Resuscitation 117:97, August 2017.
The final study we will look at on the topic of double sequential defibrillation goes back to 2017, by Emmerson et al. This study was another retrospective observational study of out-of-hospital arrest patients. Results are as follows:
In this study they did find some marginally better results for DSD in ROSC, however the benefits shown are marginal and did not demonstrate statistical significance. Additionally, the survival to discharge was notably worse. Overall, another negative trial for DSD.
Double Sequential Defibrillation Summary
So where does all of this leave us on the question of double sequential defibrillation? Our only pilot RCT looks promising for both the vector change and double sequential modalities, however we will have to wait to see if the larger RCT ends up substantiating these benefits.
All the prior studies we have had before this pilot RCT were pretty convincingly negative, however it is important to bear in mind the strong possibility of biases that may have entered the equation. Whether EMS was empowered to use DSD as they saw fit, or whether the data was examined retrospectively, it is well within the realm of feasibility that the sickest patients may be preferentially selected into double sequential groups. Employing this intervention as a last resort prior to calling a code seems very reasonable, and so there very well might be preferential utilization of this technique as more of a “hail Mary”. While we cannot at this time state with much evidence that DSD is providing significantly better outcomes, it mechanistically does not make much sense that it should perform substantially worse as observed in some of the above studies.
Ultimately all this is to say that there is no great answer currently as to whether DSD has benefit over standard defibrillation in refractory ventricular fibrillation patients. A lot will be riding on the full RCT in the works, which has the potential to eliminate so many of the potential biases complicating retrospective reviews.
With where the evidence stands at this time, it is important to bear in mind that the patient population in question is not only dead, but they are also dead in a manner that has failed the initial treatment algorithm. While there is insufficient data at this time to definitively state that double sequential defibrillation will improve that patient’s chance of survival, it does nevertheless seem reasonable to attempt it in a patient who has quickly run out of other options. After all, there are a host of case reports of this intervention being successful. With my typing the introduction above, another anecdote is added to the online body of successful stories of double sequential defibrillation. It very well may be that someday in the future one of your patients will become the latest life saved by double sequential defibrillation. But for now, it is safe to say that as of yet we are far from having sufficient evidence that this should become standard of care or that forgoing this treatment in a resuscitation is incorrect.
References
Lanan B, King M, Baker R. A Double Sequential External Defibrillation Review and Discussion. 2016; 12:41 https://www.jems.com/2016/11/30/a-double-sequential-external-defibrillation-review-and-discussion/
Cheskes S, Dorian P, Feldman M, et al. Double sequential external defibrillation for refractory ventricular fibrillation: The DOSE VF pilot randomized controlled trial. Resuscitation. 2020;150, 178‐184. doi:10.1016/j.resuscitation.2020.02.010
Lauren R. Beck, Daniel G. Ostermayer, Joseph N. Ponce, Saranya Srinivasan & Henry E. Wang (2019) Effectiveness of Prehospital Dual Sequential Defibrillation for Refractory Ventricular Fibrillation and Ventricular Tachycardia Cardiac Arrest, Prehospital Emergency Care, 23:5, 597-602, DOI: 10.1080/10903127.2019.1584256
Mapp JG, Hans AJ, Darrington AM, et al. Prehospital double sequential defibrillation: a matched case-control study. Acad Emerg Med. 2019;26(9):994-1001.
Cheskes S, Wudwud A, Turner L, et al. The impact of double sequential external defibrillation on termination of refractory ventricular fibrillation during out-of-hospital cardiac arrest. Resuscitation. 2019;139:275-281
Emmerson, A.C., et al. Double Sequential Defibrillation Therapy For Out-of-Hospital Cardiac Arrests: The London Experience. Resuscitation 117:97, August 2017
About the Author
Dr. Michael Weaver is an emergency medicine resident at USF (Class of 2022). He grew up in Saint Louis and completed medical school at the University of Missouri. Tampa is the first place he’s lived outside Missouri and he doesn’t miss winter one bit.
Post edited by Dr. Enola Okonkwo